In the treatment of malignant disease, the most important goal is treating and eradicating the cancer. Breast reconstruction is a different matter—it is a matter of what the patient envisions for the future. A motivated patient who desires a Washington DC breast reconstruction is always the is the best candidate. It can be a positive factor in a very stressful situation: Reconstruction has been found to improve self-image and self-esteem and help a woman resume her normal routines with her breasts restored to a natural look.
Advances in Breast Reconstruction
Breast reconstruction techniques have advanced dramatically over the past fifteen years. Today, many options are available, and the cosmetic results are impressive:
- Some reconstructions use breast implants and tissue expanders.
- Others use the woman’s own tissues, in the form of muscle and skin flaps (called myocutaneous flaps) with implants.
- Still others use the patient’s own tissue without implants.
This last form of breast reconstruction is called autologous reconstruction. The tissue for autologous reconstruction usually comes from the abdomen. This technique is customized to the individual patient’s needs and desires.
Breast Reconstruction Limitations
The vast majority of women who have had reconstruction surgery are pleased with their results, but there are limitations to what can be accomplished. For example:
- Surgeons cannot exactly match the other breast, although results of surgery today are coming close. To make the two breasts more closely resemble each other, some women choose to alter the unaffected breast with procedures such as reduction, augmentation (enlargement), and lift (mastopexy).
- Because a mastectomy interrupts the nerve supply to the skin, all reconstructed breasts will have less sensation in the skin, and part of this sensory change is lasting.
- All reconstructed breasts have scars, although they typically fade over time.
- Reconstructed nipples look normal, but they do not change with stimulation and appear to be always erect.
Basic Concepts
-
The Envelope and the Contents
Two concepts in breast reconstruction are:
- First, that the skin is considered an envelope; and
- Second, that the breast tissue is considered the contents.
When a patient has a mastectomy, the general surgeon removes the nipple, the biopsy site, and the contents of the breast. The usual desired goal when a woman has chosen to have breast reconstruction is a skin-sparing mastectomy. This technique involves removing the contents but attempting to limit the skin excision.
-
Restoring the Contents
All women having reconstructive surgery will require restoring breast volume after undergoing a mastectomy. A physical examination before the mastectomy determines whether there will be enough envelope remaining in which to recreate volume. If not, the patient will need additional skin for their Washington D.C. breast reconstruction procedure.
-
Measuring the Envelope
Measurements are taken during the examination to compare the normal breast to the breast with cancer. Because the nipple will be removed, the diameter of the nipple is subtracted from the vertical measurement. (If the cancer involves the skin, this skin—or envelope—is subtracted from the measurement as well; see Figure 12.1.)
Whether a patient will require additional skin (and how much) is determined by the difference between the size of the vertical skin envelope of the normal side and the anticipated vertical skin envelope after the mastectomy. The amount of skin required will play a major role in the choice of reconstruction procedure. Table 12.1 is an algorithm showing the options available to a woman needing between one and seven (or more) centimeters of additional envelope. (These procedures are described in this chapter.)
-
Figure 12.1
Modifying the Opposite Breast
As noted earlier, for some women the best result is obtained when the opposite breast is modified, as well as the breast that has undergone mastectomy. If the cancer-free breast is noticeably larger than the reconstructed breast, then the reduction of the healthy breast may be needed.
If the healthy breast droops in comparison to the reconstructed breast, then a breast lift can be performed to create symmetry. Both procedures reduce the skin envelope and could avoid the need for additional skin on the mastectomy side to achieve a symmetrical appearance.
Timing
The next issue to be considered is timing. Breast reconstruction is classified as either immediate or delayed.
- In immediate breast reconstruction in Washington, D.C., the new breast is reconstructed at the time of the mastectomy. Once the surgeon has completed the mastectomy, the plastic surgeon begins the reconstruction as part of the same operative experience.
- In delayed reconstruction, the operation may take place months or years after the mastectomy.
Delayed reconstruction and immediate reconstruction use the same techniques and have similar cosmetic results. Timing, then, is an issue of personal preference with no wrong answer and can also be a result of the woman requiring further cancer treatment after a mastectomy.
Stages in Breast Reconstruction
Breast reconstruction typically requires three steps or stages.
First Stage
The initial reconstruction with mastectomy (if immediate) or without mastectomy (if delayed) requires a general anesthetic and a one to three-day hospital stay followed by a three to four-week recovery. The other breast may be altered for symmetry at this time or could take place during the second stage.

Second Stage
The second stage is a fine-tuning or adjustment. It is performed as an outpatient procedure with a weekend recovery in most cases. The second stage takes place when two criteria are met:
- First, the patient is back to her normal routine; and
- Second, she has completed any adjuvant chemotherapy or radiation therapy.
If chemotherapy is to be followed by radiation therapy, the second stage is delayed six months to a year to enable the tissues to recover from radiation. After radiation, blood supply to the tissues is diminished, and the actual texture of the skin may be affected. The tissues are evaluated, and the timing is set on an individual basis.
The second stage includes:
- Revision of the unaffected breast for symmetry. If one side is larger than the other or one breast sits lower than the other, asymmetry can be corrected.
- If a tissue expander (a temporary implant) was placed in the initial procedure, it is exchanged for the more permanent implant at the second stage.
- Finally, if a patient elects to have a nipple reconstruction, it is started at this time. The nipple has two components, the raised part, or papule, and the pigmented area surrounding it, called the areola. The papule is created at the fine-tuning surgery.
Implant Reconstruction
One form of breast reconstruction involves breast implants. The implant is placed in a pocket that is developed under the muscles of the chest, called the pectoralis major, the serratus anterior, and the rectus abdominis. These muscles make up the layer of muscles just beneath the breast tissue.
-
Alloderm
A new addition to implant/expander reconstruction is Alloderm. This is a sheet of cadaveric dermis, derived from human skin, which is placed between the pectoralis major and the fold beneath the breast, eliminating the need to lift the certain muscles. This allows for easier expansion and in some cases the opportunity to place the actual implant at the time of the mastectomy.
Alloderm is quite exciting, as it allows for the ingrowth of blood vessels and actually becomes a part of the patient’s tissues. If the tissues are tight, an expander is placed. In smaller-breasted women, the pocket may be sufficient to accommodate the implant at the initial procedure, although this approach is less common.
-
Tissue Expanders
Moderate to large breasted women require a tissue expander to stretch the muscle and/or skin to make room for the actual implant. The tissue expander is a deflated balloon made of silicone with a built-in injection port. During the months following this reconstruction, the patient visits our plastic surgeon each one to two weeks, and the expander is inflated by injecting saline through the skin into the port, gradually inflating the expander.
This process causes little or no discomfort. The expander is inflated for several months and then removed. The permanent implant is placed as part of the second stage, the fine-tuning stage.
-
Becker Implant
An alternative to this approach is an expander/implant referred to as a Becker implant. This implant has a remote valve and can be used as an expander. Then, at the time of nipple reconstruction, the valve is removed, and the implant is left in place (see Figure 12.2).
-
Figure 12.2
Advantages of Tissue Expander-Implant Reconstruction
There are advantages of a tissue expander-implant approach over a flap approach (see below), including shorter operating time and a less involved procedure, limited to the breast area. This decreases the postoperative discomfort and recovery time. The limiting factor with tissue expansion is that only two to three centimeters of additional skin can be obtained through this technique. If more skin is required, the use of flaps is most likely appropriate as an option.
Disadvantages of Tissue Expander-Implant Reconstruction
Disadvantages associated with the tissue expander-implant option include:
- Infection, rupture, or leakage of the expander or implant;
- Contour irregularities;
- Frequent visits to the plastic surgeon in the postoperative period for expansion;
- Formation of a capsule or scar tissue around the implant, which may cause discomfort or distortion; and
- No change of implant size with weight loss or gain.
Capsular Contracture
Whenever a foreign object is placed in the body (in this case, the expander or implant), the body perceives the object as foreign and forms a wall of scar tissue around it. This scar tissue is termed a capsule. In approximately 20 percent of patients with implants, the capsule may tighten around the implant, causing discomfort and possibly a change in shape, which is termed a capsular contracture. Additional surgery may be necessary to interrupt or remove this scar tissue and possibly replace the implant. Capsular contracture may develop at any time from several months to several years following implant placement.
Schedule a Consultation
Myocutaneous Flaps
An alternative approach to breast reconstruction utilizes the patient’s own tissues, with or without an implant.
Latissimus Dorsi Flap
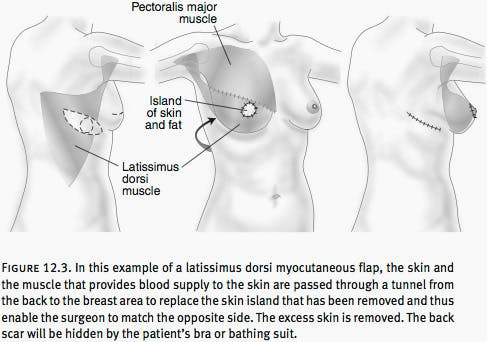
One surgical approach uses a latissimus dorsi myocutaneous flap. This is a triangular muscle from the back which is taken, along with an overlying island of skin and fat, and rotated beneath the armpit to provide the necessary skin for women requiring as much as seven to nine centimeters to be added. Depending on the size of the breast to be reconstructed, an implant may or may not be required. There are at least two additional muscles that provide each of the functions provided by the muscles and tissue moved to create breasts, and you will not notice any loss of function when this muscle is used in a flap (see Figure 12.3).
TRAM Flap
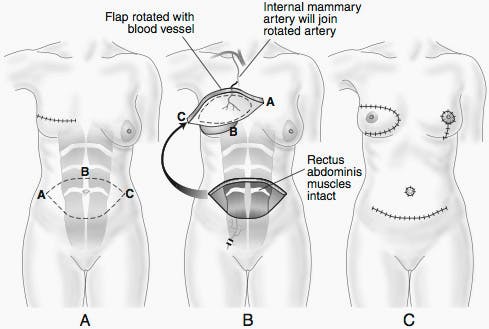
Another approach using a woman’s own tissues is the transverse rectus abdominis myocutaneous flap, or TRAM flap (see Figure 12.4). This flap employs the lower abdominal tissues that would normally be discarded if a tummy tuck were performed. These tissues are left attached to either one or both rectus abdominis muscles, which run from the center of the rib cage toward the pubic bone and are the width of a man’s tie.
The tissues form an ellipse of skin, which includes fat and muscle. This ellipse is then rotated and placed into the mastectomy defect and the skin and fat are contoured to match the opposite breast. The donor site is closed, leaving an incision line that extends across the lower abdomen from one hip to the other, with an additional scar around the navel, as are used in a tummy tuck.

Advantages of a TRAM Flap
The TRAM approach has several advantages:
- First, the TRAM utilizes the patient’s own tissues and thus avoids any issues associated with breast implants.
- In addition, the breast mound is constructed immediately after the mastectomy, avoiding the need to make frequent trips to the doctor’s office.
- The TRAM flap will shrink approximately 10 percent after surgery. The flap will change somewhat in size with associated changes in body weight gain or loss. As one ages, the breast glandular tissue is replaced with fatty tissue. Thus, the consistency of the reconstructed breast is similar to the breast on the unoperated side.
Disadvantages of a TRAM Flap
The TRAM flap also has disadvantages:
Approximately five to 10 percent of patients will lose a portion of their flap due to circulation problems, which will be noticed as an area of firmness in the flap. This area is removed at the time of the fine-tuning. There are rare reports of the entire flap being lost due to the same circulatory problems. If this occurs, the flap must be removed, and an alternative method of reconstruction chosen. For women without significant heart, lung, or vascular disease, these procedures are routinely performed without difficulties or problems.
Approximately two percent of TRAM flap patients develop a small area of abdominal wall weakness at the donor site. This is more common in cases in which both muscles are utilized. As a preventive measure, a layer of synthetic mesh may help reinforce the abdominal wall in cases where both muscles are used and in areas that may be exceptionally weak.
If this weakness occurs and the woman is uncomfortable despite wearing supportive garments, a surgical procedure is required for repair. Rarely, and more commonly when parts of both muscles are used in a case of bilateral reconstruction, the woman may have difficulty sitting up from a lying-down position. The role of the rectus muscles is to initiate the process of sitting from a lying-down position. When both muscles are used, the abdominal wall may have a temporary or permanent weakness.
DIEP Flap
One option may be to utilize the same abdominal tissues involved in the TRAM flap but leave the underlying muscle alone, avoiding the issues of abdominal wall weakness. This procedure is called a deep inferior epigastric flap or DIEP flap (see Figure 12.5). The blood vessels to the flap are dissected through the muscle and preserved, then attached to the island of skin and fat. This is called a free flap. A free flap involves cutting the blood vessels to the island of skin and then transferring the island to the chest region and attaching the blood vessel with the assistance of a microscope to local blood vessels in the chest region.
Inferior Gluteal Free Flap
Another form of free flap breast reconstruction, called the inferior gluteal free flap, employs tissues from the lower buttock (see Figure 12.6). This method fully removes an island of skin, fat, and muscle from the lower buttock, centered on the fold. The island is then transferred to the mastectomy site, where the artery and veins are connected to vessels in the armpit using the operating microscope. The advantage of this procedure is that it provides an alternative when the abdominal tissues are not available.
Disadvantages include the creation of an asymmetry in the buttock area (unless the procedure is used for bilateral breast reconstruction). There is also the potential for paresthesia, which are abnormal sensations on the back of the thigh. This procedure takes longer, typically six to eight hours, and technically is more difficult. In very rare cases, the entire flap or a portion of the flap does not survive the transfer, requiring correction surgery.

Nipple Reconstruction
Many patients choose to undergo nipple reconstruction, which is performed at the time of the fine-tuning (see Figure 12.7). As noted above, the nipple has two components:
- The raised part of the nipple, or papule, and
- The pigmented area surrounding this raised part, called the areola.

Creating the Papule
The papule is developed from the local tissues of the reconstructed breast. It is intentionally made too large, as it will compress approximately 50 percent over the six to eight weeks following nipple reconstruction. A small skin graft may be required to fill the donor site for the papule. This is typically taken from an area of redundancy on the chest wall or the ends of an existing scar.
In the past, skin grafts were taken from the groin or labial areas, but this is an older technique, no longer used. If a woman has a large papule on the other breast, a portion of that papule may be utilized to create the papule on the side of the reconstruction.
Creating the Areola
Six to eight weeks following creation of the papule, the areola is created by tattoo and the papule is also tattooed. In the majority of cases, no anesthesia is required for this in-office procedure.
Nipple Reconstruction -- Or Not
Nipple reconstruction is strictly a matter of patient preference. Although many patients choose to undergo this procedure, some do not. Before nipple reconstruction, patients tend to pay attention to their other reconstruction scars. After the nipple reconstruction, their focus is on the nipple, and the scars become less of an issue.
The Other Breast
As previously noted, a woman may decide to alter the cancer-free breast to achieve greater symmetry between the two breasts. The alteration may involve prophylactic mastectomy, enlargement, reduction, or lift. For some women, these alternatives represent the most effective means of achieving symmetry. The surgery can be performed at the time of the initial reconstruction or at the fine-tuning.
Alteration in the opposite side can help limit the amount of skin necessary to achieve symmetry in the reconstruction. A federal law states that, for insurance purposes, both breast reconstruction and alteration of the opposite side to achieve symmetry are covered procedures.
Sex and Well Being
Some women neither desire nor seek breast reconstruction after mastectomy. They resume their lives and adjust just fine. For some women, however, breast reconstruction provides an opportunity to feel whole and like themselves after mastectomy. Results of breast reconstruction allow a woman to not be reminded on a daily basis that she has had a mastectomy or cancer.
She feels comfortable wearing any clothes and getting undressed in front of her spouse or others. She can resume a normal sex life without being self-conscious. (Because the reconstructed breast has less feeling than the other breast, or no feeling, she will need to communicate with her significant other to provide a satisfying sexual experience for both.)
BRCA Gene Positive
A woman with a strong family history of breast cancer may elect to undergo gene testing. If she has a positive BRCA gene, she may have up to an 80 percent lifetime chance of developing a breast cancer. Such a woman may feel as if she is walking around with a “time bomb” and may decide to undergo bilateral prophylactic mastectomies with immediate reconstruction.
Depending on the size of the breast tissue envelope, she may have either expander-implant reconstruction or bilateral latissimus dorsi myocutaneous flaps with implant placement.
Nipple Sparing Mastectomy
Nipple sparing mastectomy is an enhanced surgical procedure that improves the outcome for women undergoing breast removal due to cancer or as a preventative measure (mastectomy). Through a small incision, the breast glandular tissue is removed from beneath the overlying skin and nipple. The breast skin envelope and nipple are left completely intact. This allows women to retain their natural nipple and that cosmetic aspect of their breasts.
Pre-pectoral Implant Placement
Pre-pectoral breast reconstruction is an excellent technique for post-mastectomy reconstruction. It allows for full preservation of the patient’s pectoralis muscle and chest wall, while also reducing pain, animation deformity, and also producing optimum patient satisfaction. The aesthetic enhancement of results requires routine use of oversizing implants in the skin envelope, careful selection of breast implants, or autologous fat grafting. With this technique, patients in all clinical scenarios can benefit from the full muscle-sparing technique of pre-pectoral breast reconstruction.
ALCL
ALCL, anaplastic large-cell lymphoma, is a cancer of the immune system which, in rare cases, affects women with breast implants. The link between implants and ALCL first came to light in 2011, with further research confirming that the rate ALCL was higher in women with breast implants. In March 2017, the FDA officially reported that breast implants could trigger the development of ALCL.
Symptoms of BIA-ALCL (breast implant associated ALCL) do not typically appear immediately, but over time. The symptoms may include:
- Pain
- Lumps
- Swelling
- Asymmetry
Testing for ALCL
To identify ALCL requires testing the fluid collected around the implant. This fluid, called a “seroma,” is not caused by ALCL, but is where the cancer cells, if present, can be identified. ALCL, when in the breast, is not a breast cancer, but a cancer of the immune system.
As reported by the FDA, ALCL is a type of non-Hodgkin’s lymphoma, or T-cell lymphoma. It is believed at this time that the risk of developing ALCL is higher in women with implants that have textured surfaces. At this time, it is considered that the development of ALCL may be triggered by chronic inflammation via bacterial infection.
Testing requires a multidisciplinary approach, including standard culture and cytological evaluation, along with other tests performed to exclude regional or systemic spread. With a complete removal of the implant and capsule when ALCL is diagnosed early, the prognosis for a full recovery appears to be excellent. Many women are choosing to have breast implants removed and come to Plastic Surgery Institute of Washington to undergo this important procedure.
Treating ALCL
To treat ALCL involves removing the implant and scar tissue that surrounds it, a procedure technically termed a capsulectomy. ALCL is a rare condition but should be treated immediately once diagnosed. If you have concerns about developing ALCL, have textured implants, or symptoms that concern you, PSIW can help. ALCL is, in the majority of cases, confined to the implant capsule, and once the implant and capsule are fully removed, good health is restored.
Plastic Surgery Institute of Washington: Breast implant removal
Our team of plastic surgeons at PSIW are each board certified by the American Board of Plastic Surgery and serve as the regions’ premier plastic and reconstructive surgeons. If you have concerns about developing ALCL, we can assist you to remove breast implants and restore your natural breast tissue and reshape an aesthetically-appealing breast mound.
Your health and breast implants
While ALCL is a rare condition, you may have health concerns, particularly if your breasts were augmented with textured surface implants. Allergen, the developer of the most popular textured breast implants has suspended sales of these implants in Europe pending further studies.
Following breast augmentation surgery, it is normal to experience swelling and discomfort as the body heals and should not be cause for concern. Once you have fully recovered from surgery, if you notice any unusual swelling or pain around the implant or other changes, testing for ALCL should be performed.
Take your first step on a journey to a new you.








